What is Aortic Stenosis?
Aortic stenosis is a progressive disease that occurs with a narrowing of the patient’s aortic valve opening. Aortic stenosis primarily happens over time as we age but can also be caused by a birth defect, previous chest radiation, or rheumatic fever. It’s typically measured as mild, moderate, or severe aortic stenosis. As a result of the reduced blood flow, the body does not get the oxygen it needs, which may cause symptoms.
Symptoms of this condition include chest discomfort or pain, shortness of breath, leg swelling, fatigue, or fainting. Left untreated, the heart muscle can weaken over time resulting in worsening of symptoms and premature death.
Treatment Options for Aortic Stenosis
- Medical/Pharmaceutical Treatment – certain medications may be prescribed to alleviate some of the symptoms of aortic stenosis, but do not stop the progression of the disease.
- SAVR (Surgical Aortic Valve Replacement) – the aortic valve is replaced through a surgical incision on the front of the chest.
- Balloon Aortic Valvuloplasty – a balloon is inserted into the aortic valve through a catheter which temporarily enlarges the valve opening.
The best treatment decision for aortic stenosis is patient specific and based on several factors including disease progression. Please consult with your provider for more information.
Possible Complications
Below is a list of possible complications of valve replacement:
- Infection
- Bleeding
- Irregular heart rhythms
- Scarring
- Blood clot formation resulting in stroke or kidney damage
- New valve functionality complications
- Complications from anesthesia
Risk factors that may increase the likelihood of complications include:
- Other heart conditions
- Lung conditions
- Chronic illness, including high blood pressure and diabetes
- Increased age
- Infections
- Smoking
- Obesity
Planning for the TAVR Procedure
Prior to the Procedure
Before your procedure at Sharon Regional, you will meet with a treatment team to discuss your history and symptoms. You will likely be referred for further testing to determine if the TAVR procedure is the right option for you. This testing may include:
- Cardiac Catherization – a small catheter is threaded into your heart from a blood vessel in your arm or leg to obtain images of your coronary arteries.
- Computerized Tomography (CT) of your chest, abdomen, and pelvis. Contrast solution is injected into a vein followed by a CT scan with images to determine the best approach and valve size.
Consult with your doctor about your current medications. You may need to stop taking certain medications at least one week prior to the procedure, such as:
- Certain diabetes medications, such as metformin (Glucophage)
- Blood thinners, such as warfarin (Coumadin)
- Anti-platelets, such as clopidogrel (Plavix)
Your physician or treatment team may ask you to:
- Not eat or drink anything after midnight the day before the procedure.
- Arrange for transportation to and from the hospital.
- Arrange for help at home after discharge from the hospital.
During the Procedure
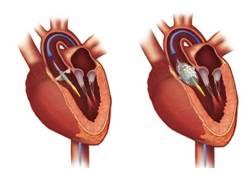 The most common approach for the TAVR procedure is transfemoral – the catheter is inserted through the artery in your groin area and is carefully passed up into the heart. The new valve is implanted through this catheter inside the narrowed aortic valve.
The most common approach for the TAVR procedure is transfemoral – the catheter is inserted through the artery in your groin area and is carefully passed up into the heart. The new valve is implanted through this catheter inside the narrowed aortic valve.
The procedure will take approximately 2 to 4 hours.
Anesthesia is used during the procedure to block pain.
After the Procedure
You will be monitored in Sharon Regional’s Cardiac Intensive Care Unit after the procedure. When you awake you will notice you are attached to several monitoring devices, which may include:
- Monitors to track heart rate, breathing, blood pressure and the percentage of oxygen in your blood stream
- A catheter in your bladder to drain urine
- An IV to provide fluids, electrolytes, and pain medications directly through a vein
In our Cardiac ICU you will be cared for by skilled critical care physicians, advanced practitioners, nurses, therapists, and technicians. The postoperative care team will assist you with coughing, deep breathing, and getting out of bed. These are important exercises for your recovery. You may be discharged directly from the Cardiac ICU or will move to another hospital bed, if needed, for continued recovery.
The current average hospital stay after the TAVR procedure is one night, but the length of stay will be dependent on your overall health and recovery progress.
Recovering after the TAVR Procedure
It is important to remember that full recovery from your TAVR procedure will take time. Most patients will see improvement of symptoms within one week, but some may make faster or slower progress depending on their overall health.
A follow-up appointment will be made about a week after your procedure.
In case of an emergency, call 911 and seek medical help right away.
More information about the TAVR procedure can be found at www.NewHeartValve.com.